
Explain the process of external respiration.
Answer
526.8k+ views
Hint: External respiration is the formal term for the exchange of gas. It describes both the mass flow of air into and out of the lungs and the transfer of oxygen and carbon dioxide into the bloodstream through diffusion.
Complete answer:
The respiratory system, also known as pulmonary ventilation, aids in breathing. Air is inhaled through the nasal and oral cavities during pulmonary ventilation (the nose and mouth). It travels into the lungs via the pharynx, larynx, and trachea. The air is then exhaled, returning through the same pathway.
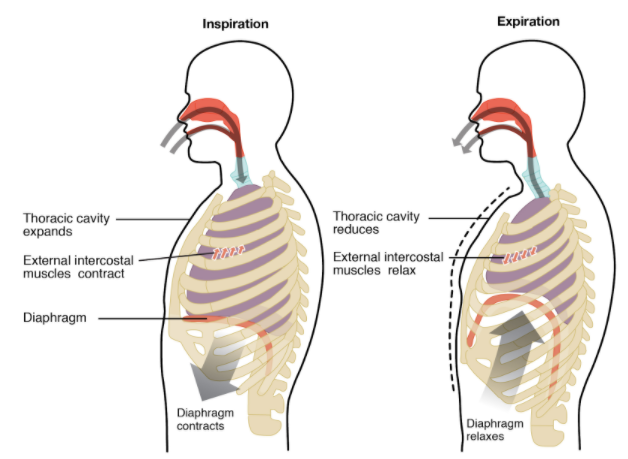
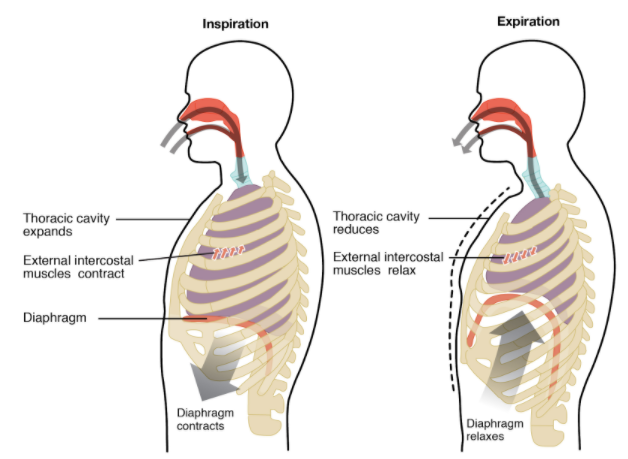
Pulmonary ventilation is triggered by changes in the volume and pressure of the lungs. The diaphragm and external intercostal muscles contract and the ribcage elevates during normal inhalation. As the volume of the lungs expands, air pressure falls and more air rushes in. Muscles relax during normal exhalation. The lungs contract, air pressure rises, and air is expelled.
Through a process known as external respiration, oxygen is exchanged for carbon dioxide waste inside the lungs. This respiratory process is carried out by hundreds of millions of microscopic sacs known as alveoli. Oxygen from the inhaled air diffuses into the pulmonary capillaries that surround the alveoli.
It binds to haemoglobin molecules in red blood cells and circulates in the bloodstream. Meanwhile, carbon dioxide from deoxygenated blood diffuses into the alveoli and is expelled through exhalation.
External respiration is the formal term for the exchange of gas. It describes both the mass flow of air into and out of the lungs and the transfer of oxygen and carbon dioxide into the bloodstream through diffusion. While the bulk air flow from the external environment is due to pressure changes in the lungs, the mechanisms for the exchange of alveolar gas are more complicated.
The primary three components of external respiration are the surface area of the alveolar membrane, the partial pressure gradients of the gases and the combination of perfusion and ventilation.
Surface Area: Alveoli have a very high surface area-to-volume ratio that allows for efficient gas exchange. Alveoli are covered by a high density of capillaries that provide many gas exchange sites.
The walls of the alveolar membrane are thin and covered with a fluid, extracellular matrix that provides the surface for gas molecules to be diffused into the air of the lungs, from which they can then be diffused into the capillaries.
Partial Pressure Gradients: Partial pressure gradients (differences in partial pressure) allow oxygen to be charged to the bloodstream and carbon dioxide to be discharged from the bloodstream. These two processes are taking place at the same time.
Oxygen has a partial pressure gradient of about 60 mmHg (100 mmHg in alveolar air and 40 mmHg in deoxygenated blood) and spreads rapidly from alveolar air to the capillary.
The balance between the alveolar air and the capillaries is reached quickly, within the first third of the capillary length within a third of a second.
Partial oxygen pressure in the capillary oxygenated blood after oxygen loading is approximately 100 mmHg. The carbon dioxide process is similar. The partial pressure gradient for carbon dioxide is much lower than for oxygen, with only 5 mmHg (45 mmHg in deoxygenated blood and 40 mmHg in alveolar air).
Ventilation: The exchange of gas and blood supply to the lungs must be balanced in order to facilitate effective external respiration. While severe ventilation–perfusion mismatch indicates severe lung disease, minor imbalances may be corrected by maintaining an air flow that is proportional to the capillary blood flow, which maintains the balance of ventilation and perfusion.
Note: According to Henry's law, the higher solubility of carbon dioxide in the blood compared to oxygen means that, despite the lower partial pressure gradient, diffusion will still occur very quickly. Equilibrium between the alveolar air and the carbon dioxide capillaries is reached within half a second of the length of the capillaries. Partial carbon dioxide pressure in the blood leaving the capillary is 40mmHg
Complete answer:
The respiratory system, also known as pulmonary ventilation, aids in breathing. Air is inhaled through the nasal and oral cavities during pulmonary ventilation (the nose and mouth). It travels into the lungs via the pharynx, larynx, and trachea. The air is then exhaled, returning through the same pathway.
Pulmonary ventilation is triggered by changes in the volume and pressure of the lungs. The diaphragm and external intercostal muscles contract and the ribcage elevates during normal inhalation. As the volume of the lungs expands, air pressure falls and more air rushes in. Muscles relax during normal exhalation. The lungs contract, air pressure rises, and air is expelled.
Through a process known as external respiration, oxygen is exchanged for carbon dioxide waste inside the lungs. This respiratory process is carried out by hundreds of millions of microscopic sacs known as alveoli. Oxygen from the inhaled air diffuses into the pulmonary capillaries that surround the alveoli.
It binds to haemoglobin molecules in red blood cells and circulates in the bloodstream. Meanwhile, carbon dioxide from deoxygenated blood diffuses into the alveoli and is expelled through exhalation.
External respiration is the formal term for the exchange of gas. It describes both the mass flow of air into and out of the lungs and the transfer of oxygen and carbon dioxide into the bloodstream through diffusion. While the bulk air flow from the external environment is due to pressure changes in the lungs, the mechanisms for the exchange of alveolar gas are more complicated.
The primary three components of external respiration are the surface area of the alveolar membrane, the partial pressure gradients of the gases and the combination of perfusion and ventilation.
Surface Area: Alveoli have a very high surface area-to-volume ratio that allows for efficient gas exchange. Alveoli are covered by a high density of capillaries that provide many gas exchange sites.
The walls of the alveolar membrane are thin and covered with a fluid, extracellular matrix that provides the surface for gas molecules to be diffused into the air of the lungs, from which they can then be diffused into the capillaries.
Partial Pressure Gradients: Partial pressure gradients (differences in partial pressure) allow oxygen to be charged to the bloodstream and carbon dioxide to be discharged from the bloodstream. These two processes are taking place at the same time.
Oxygen has a partial pressure gradient of about 60 mmHg (100 mmHg in alveolar air and 40 mmHg in deoxygenated blood) and spreads rapidly from alveolar air to the capillary.
The balance between the alveolar air and the capillaries is reached quickly, within the first third of the capillary length within a third of a second.
Partial oxygen pressure in the capillary oxygenated blood after oxygen loading is approximately 100 mmHg. The carbon dioxide process is similar. The partial pressure gradient for carbon dioxide is much lower than for oxygen, with only 5 mmHg (45 mmHg in deoxygenated blood and 40 mmHg in alveolar air).
Ventilation: The exchange of gas and blood supply to the lungs must be balanced in order to facilitate effective external respiration. While severe ventilation–perfusion mismatch indicates severe lung disease, minor imbalances may be corrected by maintaining an air flow that is proportional to the capillary blood flow, which maintains the balance of ventilation and perfusion.
Note: According to Henry's law, the higher solubility of carbon dioxide in the blood compared to oxygen means that, despite the lower partial pressure gradient, diffusion will still occur very quickly. Equilibrium between the alveolar air and the carbon dioxide capillaries is reached within half a second of the length of the capillaries. Partial carbon dioxide pressure in the blood leaving the capillary is 40mmHg
Recently Updated Pages
Master Class 11 Computer Science: Engaging Questions & Answers for Success

Master Class 11 Business Studies: Engaging Questions & Answers for Success

Master Class 11 Economics: Engaging Questions & Answers for Success

Master Class 11 English: Engaging Questions & Answers for Success

Master Class 11 Maths: Engaging Questions & Answers for Success

Master Class 11 Biology: Engaging Questions & Answers for Success

Trending doubts
There are 720 permutations of the digits 1 2 3 4 5 class 11 maths CBSE

Discuss the various forms of bacteria class 11 biology CBSE

Explain zero factorial class 11 maths CBSE

What organs are located on the left side of your body class 11 biology CBSE

Draw a diagram of nephron and explain its structur class 11 biology CBSE

How do I convert ms to kmh Give an example class 11 physics CBSE




