
What is Urine?
Urine is a liquid or semi-solid solution of waste produced by humans and animals due to physiological activities and also contains harmful compounds produced by excretory organs during fluid circulation. The human body frequently excretes waste in the form of urine. In the excretion process, our kidneys play a crucial role.
Urine contains both organic and inorganic substances. Examples of organic substances in urine include urea, creatinine, and uric acid. Inorganic solutes include sodium, potassium, and chloride. The presence of proteins gives it an acidic pH of roughly 6. Urobilin is principally responsible for the urine's colour in healthy individuals. In turn, urobilin is a byproduct of the breakdown of heme from haemoglobin during the apoptosis of old blood cells. This article explains the mechanism of urine formation.
Note: 👉Prepare for Your Future in Medicine with the NEET Rank and College Predictor 2024.
Mechanism of Urine Formation
Waste is often expelled by the human body in the form of urine, and urine is made in the nephron, the kidney's basic structural unit. Nephrons are important as they are the functional and structural units in the kidney. Nephrons, which filter the whole volume of blood in the body 60 times a day, are the backbone of the urinary system.
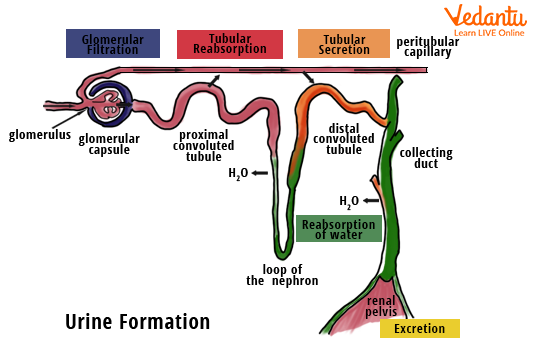
Glomerular filtration, reabsorption, and secretion are the three primary stages in the production of urine in our bodies.
Glomerular Filtration
The glomerulus is where blood is filtered. The Bowman's capsule epithelium, the endothelium of glomerular blood vessels, and the membrane between these two layers - all participate in this form of filtration.
Glomerular filtration begins when the fluid fraction of blood is filtered by the glomerulus and enters the glomerular capsule as glomerular filtrate. The filtrate is a liquid that enters the nephron after leaving the bloodstream. Except for the formed elements and plasma proteins, it encompasses all chemicals in the blood.
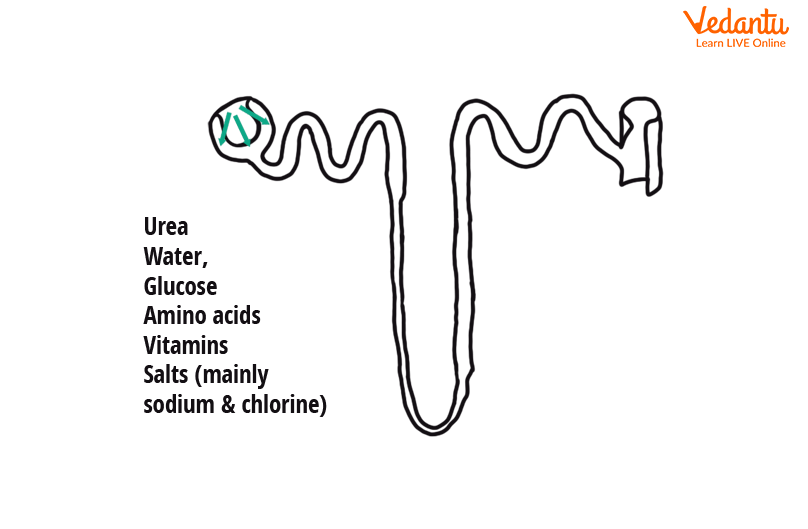
Filtration in Nephron
Water, glucose, ions, amino acids, and nitrogenous wastes are all found in this filtrate, which is collected by the renal corpuscle.
Water and other solutes are forced out of the circulation into Bowman's capsule by high blood pressure in the glomerulus. This high blood pressure is due to the afferent arteriole being more prominent than the efferent arteriole.
It is a non-energy using method (ATP).
Other capillary membranes are 1,000 times more permeable to water and solutes than the filtering membrane.
Reabsorption
The reabsorption process takes place mostly in the renal tubules (the proximal convoluted tubule (PCT), a loop of Henle, and the distal convoluted tubule (DCT). This is where 99% of the filtrate is produced. It refers to the return of substances from the filtrate (in the nephron) to the blood circulation (of peritubular capillaries). Urea, uric acid, and creatinine are nitrogenous wastes that are not reabsorbed. This is an active as well as a passive process.
The Proximal Convoluted Tubule (PCT): The proximal convoluted tubules are where the majority of reabsorption takes place. The glucose in the filtrate is reabsorbed into the blood, most of which occurs in the PCT. The Na+-K+ pump, which employs ATP, actively transports most of the sodium cations (65%) from the proximal convoluted tubules back into circulation. Amino acids and vitamins are reabsorbed into the bloodstream from the PCT.
Loop of Henle: The remaining water is reabsorbed by the descending limb. From the ascending limb, sodium ions and chloride ions are reabsorbed.
The Distal Convoluted Tubule (DCT): DCT is capable of selective reabsorption of chemicals that have remained in the filtrate. It is dependent on the body's present needs. Hormones such as aldosterone regulate it. Also, aldosterone regulates sodium ions’ reabsorption in DCT.
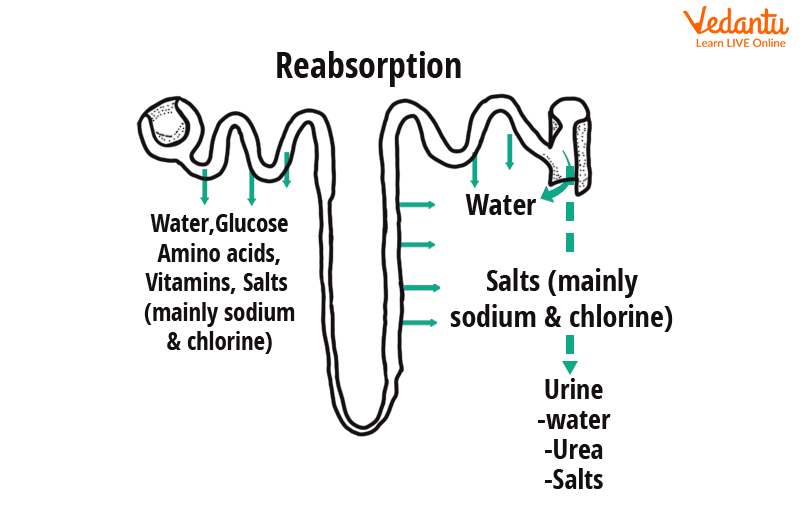
Tubular Reabsorption in The Nephron
Secretion
It includes tubular secretion. It entails adding substances to the filtrate obtained from the blood in peritubular capillaries (by active transport).
Any remaining nitrogenous wastes, some medications, and H+ ions are the main materials secreted to maintain the pH of the blood.
Tubular cells secrete hydrogen ions, potassium ions, and other ions into the filtrate.
As Na+ is reabsorbed, the potassium (K+) cation is released into DCT. The hormone aldosterone regulates K+ secretion.
The pH of the blood rises as H+ ions are released into the filtrate (it becomes less acidic).
The secretion also removes urea, uric acid, ammonium ions, and certain medicines from the blood.
Urine is the result of the fluid entering the collecting duct.
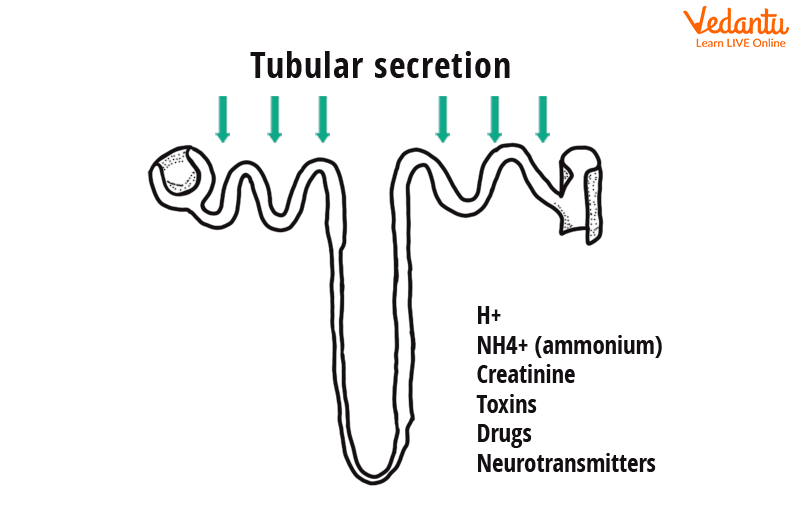
Tubular Secretion in Nephron
Mechanism of Urine Formation Diagram
The following diagram provides a clear understanding of the mechanism of urine formation and the various steps involved in it.
Urine Formation Steps
Mechanism of Urine Formation Flow Chart
The following flowchart explains the urine formation mechanism in a step-by-step manner.
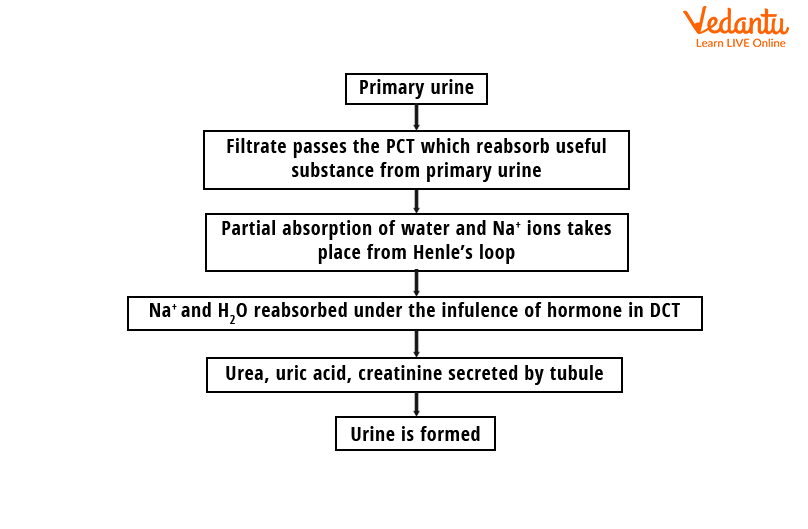
Urine Formation - Flow Chart
Countercurrent Mechanism of Urine Formation
The objective of countercurrent processes is to build and maintain an osmotic gradient of renal interstitial fluid from the renal cortex to the medulla, allowing the kidney to change the concentration of urine.
In countercurrent mechanisms, the juxtamedullary type of nephron is engaged.
The countercurrent multiplier, or countercurrent mechanism, is used by the nephrons of the mammalian urinary system to reduce the amount of water in urine by which concentrated urine is formed in the kidneys. The Loop of Henle works as a countercurrent multiplier, while the Vasa Recta maintains the gradient and acts as a countercurrent exchanger.
Countercurrent multiplication is the process by which countercurrent flow creates a steadily growing osmotic gradient in the interstitial fluid of the renal medulla.
The nephrons that produce concentrated urine run the length of the kidney, from the cortex to the medulla, and are carried by the vasa recta.
The filtrate travels in opposing ways into the two limbs of Henle's loop. Hence, the flow of blood cells in the vasa recta is similarly in opposite directions. Both the descending limb, which transports tubular fluid into the medulla and the ascending limb, which carry tubular fluid in the opposite direction, have countercurrent flow.
Solved Problems
Q1. Which of the following structures constitutes the countercurrent mechanism?
Henle’s loop and glomerulus
PCT and DCT
Henle’s loop and vasa recta
Vasa recta and collecting
Ans: (c)
The countercurrent mechanism's purpose is to produce urine with a different concentration than normal urine. The body prefers urine that is more concentrated than plasma to conserve water. The body expels excess water, and the osmolarity of urine will be lower than that of plasma. The Henle's loop of the nephron is a U-shaped segment. In the two arms of the tube, blood flows in opposite directions, generating countercurrents. In the renal medulla, the Vasa Recta is an efferent arteriole that forms a capillary network around the tubules. It is U-shaped and travels in the same direction as Henle's loop.
Q2. Which of the following is not passed on to the lumen of Bowman’s capsule during glomerular filtration?
Fat molecules
Glucose
Water
Proteins
Ans: (d)
Glomerular filtration occurs in the glomerulus of the nephron with blood flowing via the capillaries of the glomerulus to the filtrate in the glomerular capsule (Bowman's capsule). During glomerular filtration, proteins are not transmitted into the lumen of the Bowman's capsule as the blood is filtered so finely by the podocytes of the Bowman's capsule, that practically all of the plasma constituents except the proteins pass into the lumen of the Bowman's capsule. The glomerular filtration pressure is equal to the fluid pressure in the Bowman's space and osmotic force, which is owing to protein in plasma, which are the forces opposing filtration.
Conclusion
This article has given all the necessary details about the mechanism of urine formation with respect to the NEET syllabus. The questions added at the end of the article are frequently asked questions and are important from the exam point of view. Thus, the student can have a clearer understanding of the questions that might appear in the exam. Download the mechanism of urine formation PDF from our website to prepare well.
FAQs on Mechanism of Urine Formation - NEET Important Topic
1. What are the three steps of urine formation?
The human body excretes waste primarily in the form of urine. Our kidneys play a very important role in the excretion process. It occurs through 3 major renal processes that form urine:
Glomerular Filtration- Here the blood is filtered through the filtration surface of the capillaries and Bowman's capsule as the blood flows through the glomerular capillaries.
Tubular Reabsorption- In the renal tubule, almost all the filtrate (water and solute) is reabsorbed.
Tubular Secretion- Molecules are transferred from the extracellular fluid into the nephron's lumen. Drugs, creatinine and urea are all secreted.
2. What is the composition of urine?
The urine is an aqueous solution that contains more than 95 percent water and a minimum of the following constituents, in decreasing order of concentration: 9.3 g/L urea, 1.87 g/L chloride, 1.17 g/L sodium, 0.750 g/L potassium, Creatinine concentration - 0.670 g/L. Inorganic and organic compounds, as well as other dissolved ions (proteins, hormones, metabolites). Urine is sterile until it reaches the urethra, where facultatively anaerobic gram-negative rods and cocci colonise the epithelial cells lining the urethra. Unlike ammonia, which can be highly toxic to mammals, urea is essentially a processed form of ammonia. It is formed in the liver from ammonia and carbon dioxide.
3. What is dialysis?
When the kidneys stop working properly, dialysis is used to remove waste products and excess fluid from the blood. It frequently entails redirecting blood to a machine for cleaning. Hemodialysis removes excess potassium, a mineral that your kidneys normally remove from your body. Your heart may beat irregularly or stop if too much or too little potassium is removed during dialysis. While most dialysis patients will remain on it indefinitely, dialysis can be temporary in cases where the kidneys suddenly lose their ability to filter and clean your blood. Doctors may then recommend dialysis for a short period of time until your kidneys recover function.